What is Diabetes?
Diabetes is a condition where the cells in your body cant take up sugar (glucose) into its cells, resulting in an excess amount of glucose within the bloodstream.
Management of Diabetes
- Healthy eating, regular physical activity, and monitoring blood sugar levels
- Medication, such as insulin or oral diabetes drugs
- Regular check-ups, blood tests, and other medical screenings may also be necessary
- Monitor for and manage any potential complications of diabetes, such as high blood pressure and heart disease.
Hyperglycemia (Uncontrolled Diabetes)
Hyperglycemia is a condition characterized as a state where the person suffering from diabetes cannot maintain healthy blood sugar levels despite taking medication and following a diet and exercise regimen.
Hyperglycemia Signs
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Slow healing of wounds
- Dry mouth and skin
- Increased Hunger
- Numbness and tingling in the hands and feet
How to Prevent Hyperglycemia
- Maintain a healthy diet
- Regular physical activity
- Monitoring blood sugar levels
- Medication
- Avoid smoking and alcohol consumption
- Reduce stress
- Getting enough sleep
- Regular check-ups
Three Main Types of Diabetes
- Type 1 Diabetes
- Type 2 Diabetes
- Gestational Diabetes
Symptoms of Diabetes
In some cases, there may be no symptoms at all. Or you could be experiencing these symptoms;
- Increased thirst and urination
- Fatigue
- Blurred vision
- Slow healing of cuts and wounds
- Frequent infections
Early Signs of Type 1 Diabetes
- Increased thirst and urination
- Fatigue
- Blurred vision
- Rapid weight loss
- Nausea and vomiting
- Dry, itchy skin
- Slow healing of cuts and wounds
Early Signs of Type 2 Diabetes
- Increased thirst and urination
- Fatigue
- Blurred vision
- Slow healing of cuts and wounds
- Numbness or tingling in the hands and feet
- Frequent yeast infections
- Darkened skin
- Weight gain or difficulty losing weight
Early Signs of Gestational Diabetes
- Increased thirst and urination
- Fatigue
- Blurred vision
- Slow healing of cuts and wounds
- Numbness or tingling in the hands and feet
- Frequent yeast infections
- Weight gain or difficulty losing weight
How to Lower Blood Sugar Levels Naturally
- Exercise
- Manage Your Carb Intake
- Stay Hydrated
- Environmental Factors
- Overall Health
- Portion Control
- Fiber-Rich Diet
- Manage Stress Levels
- Enough Quality Sleep
- Adding Specific Foods to your Diet
Gestational Diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. It occurs when the body cannot produce enough insulin to meet the increased demands of pregnancy, leading to high blood sugar levels.
It develops around the 24th to 28th week of pregnancy but can occur earlier or later. It affects about 4% of all pregnancies.
Causes of Gestational Diabetes
- Obesity
- Previous gestational diabetes
- Polycystic ovary syndrome (PCOS)
- High blood pressure
- Impaired glucose tolerance or impaired fasting glucose prior to pregnancy
- Previous stillbirth or neonatal death
Risk Factors for Gestational Diabetes
- Family history of pre-diabetes or Type 2 diabetes
- Being overweight before your pregnancy
- Being African-American, Asian-American, Hispanic, or Native-American
- Being over 25 years of age


- ZUMEIJIA Women's Diabetic Shoes for Women Casual Adjustable Walking Shoes Wide Shoes for Elderly Swollen Feet Non-Slip Air Cushion Bottom Fattening and Widening

- CareSens N Plus Bluetooth Blood Glucose Monitor Kit with 100 Blood Sugar Test Strips

- Glucology Insulin Pump Waist Belt Fanny Pack for Running or Travel - Diabetes Supplies Pouch and Accessories for Men and Women -Slim, Discreet Design
Are you or a loved one navigating the complexities of diabetes? This chronic condition, affecting millions worldwide, requires not only medical attention but also a deep understanding of its impact on daily life. In this blog, we'll dive into the world of diabetes, exploring its types, causes, and the latest in management strategies.
From lifestyle changes to advancements in treatment, we aim to provide valuable insights for those living with diabetes. Join us as we unravel the intricacies of this condition, offering support and information to help you lead a healthier, more informed life with diabetes.
What is diabetes?
Diabetes is a long-term health issue. It changes how your body uses food for energy.
Here's how it works. Your body turns most food into sugar, called glucose. This sugar goes into your blood. When your blood sugar rises, your pancreas makes insulin. Insulin helps sugar enter your body's cells for energy.
But in diabetes, your body can't make enough insulin or use it well. Without enough insulin, or if cells don't respond to it, too much sugar stays in your blood. Over time, this can lead to big health problems, like heart disease, vision loss, and kidney disease. There's no cure for diabetes yet. But, you can manage it. Losing weight, eating healthy, and staying active help a lot.[1]
The role of insulin in the absorption of glucose
When you eat, your body breaks down food into nutrients. Carbohydrates, found in foods like pasta and bread, are turned into glucose. Glucose is a sugar that gives you energy. The pancreas makes two important chemicals, insulin and glucagon, to control how much glucose is in your blood.
Insulin helps your muscles and fat cells use glucose. When there's too much glucose, insulin lowers it. Glucagon does the opposite; it raises glucose when there's not enough. This balance is called homeostasis, keeping everything just right inside your body.
If your body can't make enough insulin, glucose builds up in your blood. This is called hyperglycemia. Keeping glucose levels balanced is important. It gives your cells energy and stops damage from too much sugar, like nerve harm.[2][3]
Diabetes in the USA
In 2021, about 29.7 million people in the US, or 8.9%, had diagnosed diabetes. This includes all ages. For children and teens under 20, 352,000 had diabetes. Most of them, 304,000, had type 1 diabetes. Among adults over 20 with diabetes, 1.7 million also used insulin. This is 5.7% of these adults. Another 3.6 million adults started using insulin within a year of finding out they had diabetes. This group makes up 12.3% of adults with diabetes.
Looking at US adults 18 and older from 2019 to 2021, we see different patterns. Diabetes was most common in American Indian and Alaska Native adults, at 13.6%. Next were non-Hispanic Black adults at 12.1%, Hispanic adults at 11.7%, non-Hispanic Asian adults at 9.1%, and non-Hispanic White adults at 6.9%.
Education level, which shows social and economic status, also affected diabetes rates. Adults with less than a high school education had a 13.1% rate of diabetes. This rate was 9.1% for those with a high school education and 6.9% for those with more education.[4]

Management of diabetes
Key aspects include balanced meal planning, understanding carbohydrates, using the plate method for portion control, and coordinating meals with medications. Exercise is crucial, with recommendations for both aerobic and strength-building activities. Regular monitoring of blood sugar levels is advised, especially in relation to exercise. Insulin and other diabetes medicines must be properly managed. The article also covers the impact of illness, alcohol consumption, hormonal changes, and stress on blood sugar levels, offering strategies for effective diabetes management in these contexts. [5]

Initial diabetes symptom and signs
Hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) are the only two initial diabetes symptoms.
Hyperglycemia (Uncontrolled Diabetes)
Hyperglycemia is when your blood has too much sugar, also known as high blood sugar. It occurs if your body lacks insulin or can't use it right. Insulin is a hormone. This condition often means you have diabetes. People with diabetes may often have hyperglycemia.
If not treated, hyperglycemia can harm your nerves, blood vessels, and other parts of your body over time. In serious cases, it can cause a dangerous problem called diabetes-related ketoacidosis (DKA). This is very serious and needs quick medical help. It's more likely in people with diabetes using insulin or those with undiagnosed Type 1 diabetes.[6]
Hyperglycemia signs
- Increased thirst
- Increased urination
- Tiredness
- Listlessness
- Nausea
- Dizziness
- Confusion
- Fatigue [7]
How to prevent hyperglycemia
- Lose extra weight
- Be more physically active
- Eat healthy plant foods
- Eat healthy fats
- Skip fad diets and make healthier choices[8]
Hypoglycemia
Hypoglycemia is when your blood sugar is too low. It means the glucose in your blood is less than normal. Often, people with diabetes have this issue if their blood sugar is under 70 milligrams per deciliter (mg/dL). But, this number can vary. So, you should talk to your doctor to know your low blood sugar level.[9]
Hypoglycemia Signs
- Sweating.
- Feeling tired.
- Dizziness.
- Feeling hungry.
- Tingling lips.
- Feeling shaky or trembling.
- Fast or pounding heartbeat
- Easily irritated, tearful, anxious, and moody.
- Turning pale.
You may also experience other symptoms if your low sugar level is not treated, such as:
- Shakiness.
- Passing out or collapsing.
- Irritability.
- Feeling sleepy.
- Blurred vision.
- Difficulty concentrating.
- Slurred speech or clumsiness.
- Passing out or collapsing.
- Seizures or fits.
- Overall Weakness.
- Confusion.[10]
A Hypo can also happen while you're sleeping. Hypo may cause you to wake up during the night. It can also cause damp sheets (from sweat), tiredness, and headaches in the morning.
How to prevent hypoglycemia
You can lower your risk of having a Hypo attack by doing the following:
- Stick to your meal plan
- Have three meals a day at regular times, with snacks if needed.
- Don't wait more than 4 to 5 hours between meals.
- Exercise 30 minutes to 1 hour after eating.
- Always check your blood sugar before and after exercise.
- Talk to your doctor about any changes.
- Make sure you're using the right amount of insulin or diabetes medicine.
- If you drink alcohol, do so in moderation and keep an eye on your blood sugar.
- Understand when your medicine works best.
- Test your blood sugar as your doctor advises.
- Always wear an ID bracelet that shows you have diabetes.[11]

Low blood sugar level if you are not a diabetic
If you have low blood glucose levels, but you, do not have diabetes,
Possible causes include:
- Diabetes medicines, including insulin
- Beta-blockers
- Sulfamethoxazole and trimethoprim (Bactrim)
- Haloperidol
- Pentamidine
- Monoamine oxidase inhibitors (MAOIs)
- Quinidine
- Sulfonylureas
- Drinking too much alcohol
- Hypothyroidism
- Side effects of weight loss surgery
- Liver or kidney problems
- Anorexia nervosa
- Problems in the pancreas
- Certain genetic disorders[12]
See a G.P. if you think you keep getting low blood sugar level symptoms. Your doctor can perform simple tests to check if your blood sugar level is low and determine what's causing it. If you keep getting a low glucose level, talk to your diabetes care team about things you can do to help prevent it.
Pre-diabetes
Many people have blood glucose levels in the normal range but not high enough to be diagnosed with diabetes.
Pre-diabetes conditions in which your blood sugar levels are higher than usual but not high enough to be classified as diabetes. If your blood glucose level is higher than the normal range, you will have an increased risk of developing diabetes. Diabetes will progressively worsen if left untreated. Diagnosis needs to happen as early as possible.

Three main types of diabetes
Type 1, Type 2, and Gestational diabetes (diabetes while pregnant).[13]
Type 1 diabetes
Type 1 diabetes happens when the body mistakenly attacks itself. This attack destroys insulin-making cells in the pancreas, known as beta cells. This damage can happen for months or even years without showing symptoms.
Certain genes increase the chance of getting type 1 diabetes. These genes are passed from parents to children. But, having these genes doesn't mean you'll definitely get diabetes. Something in the environment, like a virus, might also trigger it. Remember, your diet and lifestyle don't cause type 1 diabetes.
Type 2 diabetes
Your blood sugar level tells how much sugar is floating around in your bloodstream. This sugar is called glucose, and it's the main source of energy for your body. Normally, your blood sugar stays within a certain range. But if you have type 2 diabetes, your blood sugar levels get too high too often. This is called hyperglycemia.
It's like having a key and a lock. In a healthy body, insulin acts like the key that unlocks your cells, letting glucose in for energy. But in type 2 diabetes, either the key doesn't fit right, or the lock is broken. So, sugar gets stuck in your bloodstream instead of going where it needs to be. This is different from type 1 diabetes, where the body doesn't make any insulin at all. It's like the key factory is shut down completely.
So, type 2 diabetes is all about problems with how your body uses or makes insulin, leading to high blood sugar levels.[14]
Gestational diabetes
You might develop a type of diabetes called gestational diabetes when you're pregnant. This happens when your blood sugar gets too high, usually around the middle of pregnancy, between 24 and 28 weeks. Don't worry, having gestational diabetes doesn't mean you had diabetes before. It's caused by the pregnancy itself.[15]
Causes of gestational diabetes
Several clinical risk factors can increase the chance of getting gestational diabetes. These include:
- Being overweight, with a body mass index (BMI) over 25.
- Not being physically active.
- Having a close family member with diabetes.
- A history of gestational diabetes or having a large baby.
- Other health issues like high blood pressure.
- Low levels of good cholesterol (HDL).
- High triglycerides, especially over 250.
- Having polycystic ovarian syndrome.
- A Hemoglobin A1C level over 5.7.
- Failing an oral glucose tolerance test.
- Any sign of insulin resistance, like acanthosis nigricans.
- A past medical history of heart diseases.[16]

Diabetes risk factors are different for each type
Risk factors for type 1 diabetes
- Genetic Susceptibility: The risk is higher if a parent has type 1 diabetes, particularly in offspring of fathers with the condition. This suggests a strong genetic component.
- Environmental Factors: Increasing rates of type 1 diabetes suggest changes in environmental exposures over the past 60+ years. This could include new susceptibility factors or the loss of protective factors.
- Infectious Agents: There is a particular interest in enteroviral infections, especially those that are persistent and acquired in early childhood. The role of other infections is also considered, influenced by factors like increasing sanitation and changes in herd immunity.
- Early Childhood Diet: While early suggestions pointed to cow’s milk as a potential trigger for islet autoimmunity, this has not been confirmed in larger studies. However, various components of the early childhood diet have been associated with a 1.5–2-fold increase in risk.
- Environmental Toxins: These are being investigated as potential risk factors, though specific toxins have not been definitively linked.
- Prenatal and Early Post-natal Exposures: These time frames appear critical, as the incidence of islet autoimmunity, a precursor to type 1 diabetes, peaks in the second year of life.
- Seasonality and Geography: Outbreaks and seasonal variations in the incidence of type 1 diabetes suggest environmental factors, possibly including infectious agents, play a role.[17]
Risk Factors for Pre-Diabetes and Type 2 Diabetes
- Are overweight or obese.
- Are 35 years old or older. Kids and teens can get it too, but it's more common in older people.
- Have diabetes in your family.
- Belong to certain racial or ethnic groups. These include African American, American Indian, Asian American, Hispanic/Latino, or Pacific Islander.
- Don't move around much. This could be due to physical limits, a job that keeps you sitting a lot, or a lifestyle that doesn't include much activity.
- Have prediabetes.
- Had gestational diabetes when pregnant, or had a big baby weighing 9 pounds or more.[18]
Risk Factors for Gestational Diabetes
- Being overweight or obese.
- Not exercising or moving around much.
- Having prediabetes.
- Having had diabetes during an earlier pregnancy.
- Having polycystic ovary syndrome.
- Having a close family member with diabetes.
- Having had a big baby before, weighing more than 9 pounds (4.1 kilograms).
- Being from certain racial or ethnic groups. This includes Black, Hispanic, American Indian, and Asian American people.[19]

Symptoms of diabetes
Early Signs of Type 1 Diabetes
- Sores or cuts that heal very slowly.
- Skin that itches, often around the vaginal or groin area.
- Getting yeast infections often.
- Gaining weight recently.
- Changes in skin color and texture, like dark, velvety patches on your neck, armpit, and groin, known as acanthosis nigricans.
- Feeling numbness or tingling in your hands and feet.
- Having trouble seeing well.
- Experiencing impotence or erectile dysfunction (ED).[20]
Early Signs of Type 2 Diabetes
- Acanthosis nigricans: This is where you get darker, velvety skin. It's often on the neck, elbows, knees, and knuckles.
- Necrobiosis lipoidica: These are raised patches. They can be yellow, red, brown, or darker than your normal skin. They might swell up and get hard.
- Digital sclerosis: This is when the skin on your hands gets hard, thick, or swollen. It can also spread to your arms and other parts of your body.
- Blisters that don't hurt and appear suddenly.
- Wounds that take a long time to heal.
- Getting skin infections more often than usual.[21]
Early Signs of Gestational Diabetes
- Gestational diabetes is a condition where women develop high blood sugar levels during pregnancy. It often does not cause any symptoms initially, but as it progresses, some women may notice the following signs:
- Increased thirst
- Frequent urination
- Excessive sweating
- Fatigue
- Dry mouth
- Blurred vision
- Nausea
- Frequent bladder, vaginal, or skin infections
- It’s important to note that these symptoms are also common in pregnancy, so they can be easily overlooked. Therefore, all pregnant women are screened for gestational diabetes, usually between the 24th and 28th weeks of pregnancy23. If you notice any of these symptoms, it’s recommended to consult with your healthcare provider.[22][23]

Diagnosis
The glycated hemoglobin (A1C) test diagnoses type 1, 2, and gestational diabetes. This blood test reveals your average glucose level in your blood during the previous two to three months.
Results can be interpreted as follows:
- Below 5.7% is in the normal range.
- 5.8% to 6.4% is pre-diabetes.
- 6.5% or higher on two different tests indicates diabetes.
If the A1C test isn't accessible, or if you have any restrictions that interfere with an A1C test, your doctor may employ one of the following tests to establish diabetes:
- Random blood glucose level test.
- Fasting blood sugar test.
- Oral glucose tolerance test.
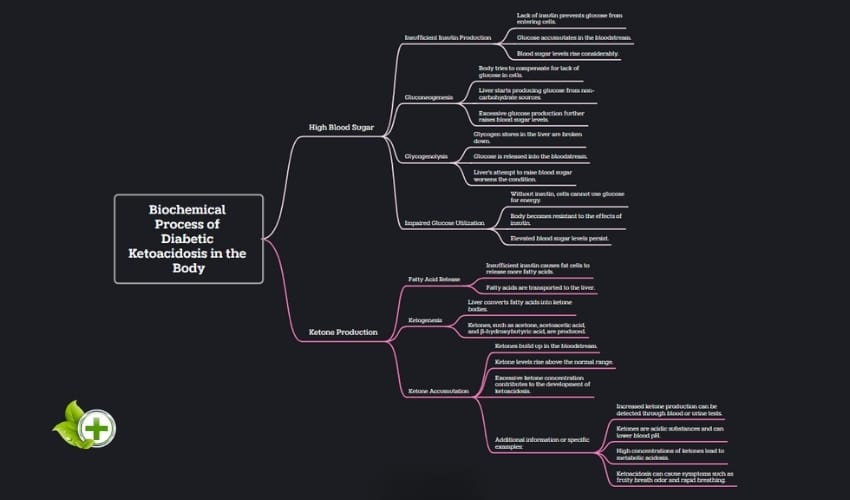
Diabetic Ketoacidosis (DKA)
Diabetic ketoacidosis, or DKA, is a dangerous diabetes problem. It happens when you don't have enough insulin. Insulin helps turn blood sugar into energy. Without it, your body uses fat for energy. This makes ketones in your blood.
Too many ketones can harm your body. They make your blood acidic. This is ketoacidosis. DKA can be deadly if you don't get help fast. Its signs develop slowly. Knowing them is key. Early discovery can prevent and treat DKA.[24]
Symptoms of DKA
- Elevated Blood Glucose Levels: Mentioning blood glucose greater than 250 mg/dl as a criterion for DKA.
- Acid-Base Imbalance: Describes arterial pH less than 7.3 and serum bicarbonate less than 15 mEq/l, indicating acidosis.
- Presence of Ketonemia or Ketonuria: Key features in the diagnosis of DKA.
- Anion Gap Metabolic Acidosis: An anion gap greater than 14-15 mEq/l is indicative of this condition.
- Leukocytosis: A common finding in DKA patients.
- Electrolyte Imbalances: Describes falsely low serum sodium, elevated serum potassium due to shifts from intracellular to extracellular spaces, low magnesium, and phosphate levels.
- Ketone Body Ratio Changes: In DKA, the ketone body ratio (3-beta-hydroxybutyrate:acetoacetate) changes significantly.
- Pancreatic Enzyme Levels: Elevated in DKA due to disorders in carbohydrate metabolism.
- Lipid Abnormalities: Mention of high plasma triglyceride and cholesterol levels before insulin treatment.
- Electrocardiogram (ECG) Findings: ECG changes due to electrolyte imbalances like hypokalemia or hyperkalemia.
- Imaging Tests: Describing the role of chest X-ray and brain imaging in the context of DKA.[25]
Causes of DKA
- DKA happens due to very high blood sugar and not enough insulin. The main causes are:
- Illness. When sick, eating and drinking less can make controlling blood sugar difficult.
- Missed insulin shots, problems with insulin pumps, or incorrect insulin doses.
- There are other reasons for DKA too:
- Heart attacks or strokes.
- Physical injuries, like from car accidents.
- Using alcohol or drugs.
- Some medications, like water pills and corticosteroids, which treat swelling in the body.[26]

Hyperosmolar hyperglycemic (HHS)
Hyperosmolar Hyperglycemic Syndrome (HHS) is a serious complication of diabetes mellitus, most commonly seen in type 2 diabetes. It is characterized by severe hyperglycemia (high blood sugar) and glycosuria (excess sugar in urine), without the typical symptoms of diabetic ketoacidosis, such as Kussmaul breathing or acetone in the urine. HHS was previously known as non-ketotic hyperglycemic coma or hyperosmolar non-ketotic coma (HONK).[27]
Symptoms of HHS
Hyperosmolar hyperglycemic can take days or weeks to develop. Possible signs and symptoms include:
- Extremely high blood sugar, above 600 mg/dL or 33 mmol/L.
- Changes in mental state, like being confused, delirious, or seeing things that aren't there.
- Passing out.
- Having a very dry mouth and feeling extremely thirsty.
- Needing to urinate often.
- Vision that's blurry or losing sight.
- Feeling weak or possibly having trouble moving, especially on one side of the body.[28]
Causes of HHS
- Not Enough Insulin: In HHS, the body still makes some insulin, but it's not enough. This is different from another diabetes problem called diabetic ketoacidosis, where there's hardly any insulin.
- Not Drinking Enough Water: If you don't drink enough water, your blood sugar can get very high. This makes HHS worse.
- Sugar Can't Get Into Muscles: When there's not enough insulin, sugar can't enter your muscles well. This makes your blood sugar go up.
- Liver Makes More Sugar: Without enough insulin, your liver makes more sugar. This adds to the high blood sugar problem.
- Body Reacts to High Sugar: Your body tries to balance the high sugar by releasing certain hormones. But these hormones actually make your blood sugar even higher.
- Losing Water Because of Sugar: When your blood sugar is very high, you pee out more sugar and water. This can make you very dehydrated.
- No Ketosis: Unlike in diabetic ketoacidosis, HHS doesn't usually lead to a condition called ketosis. This is because the little insulin that is there stops fat from breaking down too much.
- More Common in Afro-Caribbean People: Research shows that people of Afro-Caribbean descent might be more likely to get HHS.
- More Likely in Older Adults: Older people, especially those with type 2 diabetes, are more likely to develop HHS.
- Very High Blood Sugar: If your blood sugar is extremely high, you might pee out a lot of water. This can lead to severe dehydration and a very high blood sugar level.
- Water Pulled from Cells: The high sugar in your blood can pull water out of your cells. This can make dehydration worse.[29]
Consult your doctor if your blood glucose is persistently higher than the target range recommended or if you have signs or symptoms of diabetic hyperosmolar syndrome.
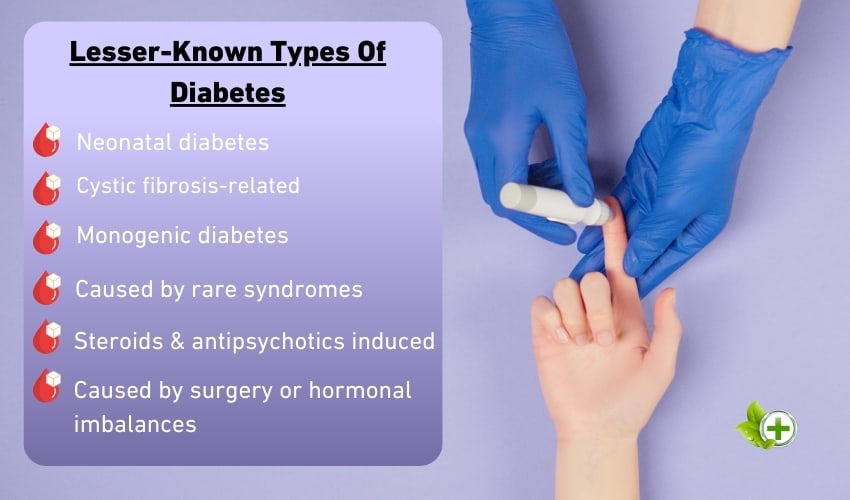
Other Types of Diabetes
Type 1, Type 2, and gestational diabetes are the main ones but there is a range of other types of diabetes. These types of diabetes are rare, with about 2% of people affected by them. These rare types of diabetes include:
- Maturity onset diabetes of the young (MODY)
- Neonatal diabetes
- Wolfram Syndrome
- Alström Syndrome
- Latent Autoimmune diabetes in Adults (LADA)
- Type 3c diabetes
- Steroid-induced diabetes
- Cystic fibrosis diabetes[30]
Unfortunately, many people with rarer types of diabetes are misdiagnosed, leading to delays in getting the proper treatment.

How to Lower Blood Sugar Levels Naturally
Blood glucose control and management are essential for people with diabetes, as chronically high blood glucose levels can lead to life threatening complications. The following are some simple and evidence-based methods for reducing blood glucose levels naturally and in addition to controlling your glucose absorption.
Exercise
Regular exercise may assist you in achieving and maintaining healthy body weight while also improving insulin sensitivity. Your cells can more easily use the available sugar in your bloodstream by increasing your insulin sensitivity.
Taking frequent sitting breaks for a few minutes is a good idea for office workers. Squatting or leg raises, for example, or simply walking are all excellent options.[31]
Manage Your Carb Intake
Complex carbs, like those in whole grains and veggies with lots of fiber, go into your blood slowly. This is good because it helps avoid quick rises in your blood sugar. But simple carbs, found in things like sweet drinks and cakes, can make your blood sugar shoot up fast.
Also, it's a good idea to spread out eating carbs during the day. This stops your body from getting too many carbs at once, which can be hard to handle. If you eat more carbs than your insulin can manage, your blood sugar might go up. If you eat too few carbs, your blood sugar might drop too low. Remember, it's always smart to talk to a doctor or a dietitian for advice that fits you. They can guide you based on your own health and way of life.[32][33]
Stay Hydrated
Drinking water can help lower your blood sugar in a few ways:
- Diluting Blood Sugar: Drinking lots of water can help thin out the sugar in your blood. This helps with blood sugar control.[34]
- Getting Rid of Sugar: Water helps your kidneys get rid of extra sugar through pee. This is really good when your blood sugar is high because it helps get more sugar out of your blood.[35]
- Stopping Dehydration: When you drink water, it helps add water back into your blood. This is important when your body is trying to get rid of sugar through pee. If you don't drink enough water, your body might take water from other places, like your saliva or tears. This can make you even more dehydrated.[36]
Remember, while water is helpful for controlling blood sugar, it's just one part of managing diabetes. You should also eat healthy, exercise, and take medicine if your doctor says so. Always talk to a doctor for advice that's right for you. Keeping your skin hydrated is also important, and you can learn more about that by reading How To Care For Dehydrated Skin.
Portion Control
Monitoring your serving sizes by implementing portion control can help you regulate your calorie intake and maintain a moderate weight.[37]
Fiber-Rich Diet
There are two types of fiber— insoluble and soluble.
- Soluble fiber dissolves in water and includes plant pectin and gums.
- Insoluble fiber doesn't dissolve in water. It provides plant cellulose and hemicellulose.
A high fiber diet minimizes blood glucose lows and improves your body's ability to regulate blood sugar levels. The recommended daily fiber intake is about 14 grams for every 1,000 calories. Foods high in fiber include fruit, vegetables, whole grains, and legumes.[38]
Manage Stress Levels
When you're stressed, your body releases hormones like cortisol and adrenaline. These hormones are meant to give you energy. This energy is for 'fight or flight' reactions. However, these hormones make it tough for insulin to do its job. This problem is called insulin resistance. Because of it, energy can't enter your cells well. So, your blood sugar levels go up.
If your blood sugar gets too high, it's known as going hyper. The full name is hyperglycaemia. We have lots of information about hypers. This includes how to prevent them and how to treat them. Stress that lasts a long time can keep your blood sugar high. This increases your risk of diabetes complications. Long-term stress can also change your mood and self-care habits. These changes can impact your emotional health.[39]
Enough Quality Sleep
It's not totally clear, but many studies show a link between sleep and diabetes. First, people who get less than 6 hours of sleep a night often eat at irregular times. They also snack more and choose unhealthy foods. This can affect blood sugar levels.
Next, not getting enough sleep changes how your body makes hormones. This can impact blood sugar too. For example, staying up late increases cortisol, a hormone. Cortisol can make insulin, another hormone, less effective. Insulin is important for controlling blood sugar.
Also, disturbing your body’s natural sleep cycle, or circadian rhythm, is bad. Being awake at night can make your body less responsive to insulin. A study showed this. In the study, 16 people only slept 5 hours each night for 5 days. When they ate at night, their bodies didn’t handle insulin well.[40]
Adding Specific Foods to your Diet
Some of the food products advertised to have anti-diabetes properties include:
- Apple cider vinegar
- Cinnamon
- Berberine
- Fenugreek seeds
- Eat chromium and magnesium-rich foods
Important: Checking your blood sugar levels and recording them in a diary helps you adapt meals and drugs as needed to control your blood sugar levels better. The Food and Drug Administration (FDA) regulates supplements differently than prescription medications. It's critical to get supplements that an independent lab has evaluated for purity and ingredient content. If you're already taking blood-sugar-lowering medications, please discuss herbal supplements with your doctor, as your medicine may negatively interact with them.
Low Glycemic Index
Different carbohydrate-containing foods affect blood sugar levels differently. These effects quantify the measurement known as the glycemic index.
What is the Glycemic Index (G.I.)?
It's how fast the carbohydrates are broken down and digested into the blood. Also, how much power and speed it has to raise your glucose level.
Glycemic index <50=Low, 50-70=Med, >70= High
If you have diabetes, your blood sugar increases when you eat carbohydrates. The number of carbs you consume at a meal or in a snack mainly determines what your blood sugar will do. The G.I. divides foods into low, medium, and high and ranks them on a scale of 0–100. On the other hand, the glycemic index provides only a portion of the picture. It doesn't tell you how high your blood sugar will rise after eating that food. To fully comprehend a food's impact on blood sugar, you must first understand how quickly glucose enters the bloodstream and how much glucose per serving it can provide.
Low glycemic Load
The glycemic load, a separate measure, does both by giving you a more accurate picture of a food's real-life effects on your blood sugar.
What is the Glycemic Load?
Glycemic load is the concentrated amount of carbohydrate or carbohydrate in food.
Glycemic load <10=Low, 10-20=Med, >20=High
Watermelon, has a glycemic index of 72. But a serving of watermelon has a low glycemic load of only 4. Choosing to eat good sources of carbs can help you control your blood sugar. The following link provides a general food list index with Glycemic indexes and loads. It will give you a more accurate picture of a food's real-life impact on your blood glucose.
Suggestion; Strive to consume foods with a Glycemic index less than 50 and a Glycemic load less than 10 on the scale. (Please discuss with your health care provider before changing your diet).
FAQ
What is diabetes mellitus?
Diabetes mellitus is more commonly known as diabetes.
What is diabetic hyperosmolar syndrome?
Diabetic hyperosmolar syndrome is a severe condition caused by extremely high blood sugar levels. It’s often triggered by illness or infection and commonly occurs in people with Type 2 diabetes.
What is insulin?
Insulin is a hormone. Its made by your pancreas that controls the amount of glucose in your circulation at any given moment.

